Bringing new life into the world is a profound journey, but for women with celiac disease in Pregnancy, it requires extra diligence. Undiagnosed or untreated celiac disease in pregnancy can result in serious complications. This in-depth guide empowers expectant mothers to navigate pregnancy safely and successfully while managing celiac disease, with a focus on early detection, smart nutrition, and expert-backed advice tailored to real-world challenges.
Understanding the Risks: Why Celiac Disease in Pregnancy Matters
Celiac disease is an autoimmune disorder where ingesting gluten, a protein found in wheat, rye, and barley, triggers immune damage to the small intestine. In pregnancy, unmanaged celiac disease can have severe consequences.
Risks include:
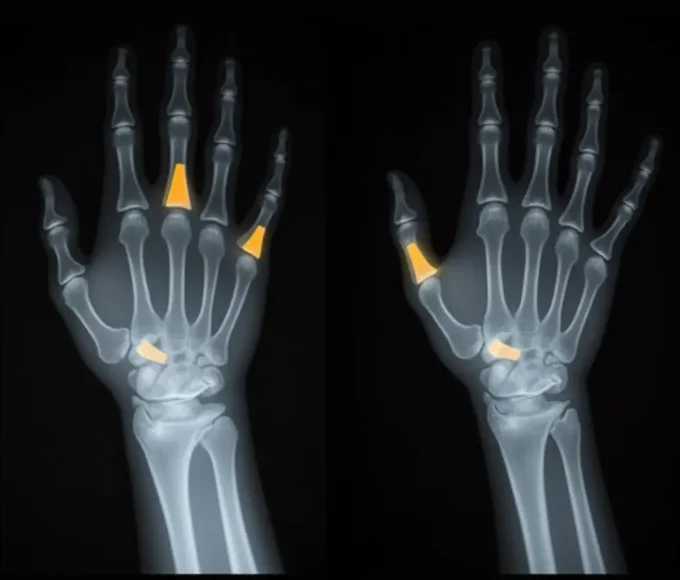
- Recurrent miscarriage or preterm labor
- Low birth weight or intrauterine growth restriction (IUGR)
- Severe maternal nutrient deficiencies, such as iron, calcium, and folate
- Unexplained infertility or difficulty conceiving
Women with known or suspected celiac disease should take proactive steps to manage their condition well before conception or as early as possible during pregnancy.
Get Diagnosed Before or During Pregnancy
Planning a pregnancy is the perfect time to rule out or confirm celiac disease in Pregnancy, especially if you’ve experienced symptoms such as bloating, chronic fatigue, frequent miscarriages, or iron-deficiency anemia. A blood test followed by an intestinal biopsy can confirm the diagnosis.
Once diagnosed, adherence to a 100% gluten-free diet becomes vital. Even minimal exposure to gluten can impair nutrient absorption, impacting fetal growth and maternal health.
Nourishing Your Pregnancy: Smart, Gluten-Free Nutrition
Pregnancy demands more nutrients, and celiac disease makes it harder for your body to absorb them. A tailored, gluten-free diet that is both calorically adequate and nutritionally rich is essential.
Key nutrients to focus on:
- Folate: Lentils, chickpeas, leafy greens, oranges
- Iron: Lean red meat, pumpkin seeds, gluten-free fortified cereals
- Calcium & Vitamin D: Dairy or fortified plant-based milk, eggs, salmon
- Vitamin B12: Eggs, meat, gluten-free nutritional yeast
Limit highly processed “gluten-free” snacks—they’re often low in fiber and high in sugar. Choose naturally gluten-free whole foods for better nourishment.
Guard Against Hidden Gluten & Cross-Contamination
Gluten hides in more places than you might expect: salad dressings, soups, soy sauce, deli meats—even some prenatal supplements.
How to protect yourself:
- Always read food and medicine labels—even if they say “gluten-free”
- Use separate cookware and utensils at home
- Educate your partner and household about cross-contamination risks
- When eating out, ask questions—request separate preparation surfaces
Navigating First Trimester Nausea
Pregnancy nausea often disrupts dietary routines. Yet, for mothers with celiac disease in Pregnancy, skipping meals or relying on unsafe convenience foods isn’t an option. Aim for small, frequent meals that are easy to digest and gentle on the stomach.
Safe, gluten-free mini-meal ideas:
- Mashed avocado on gluten-free toast
- Rice noodles with steamed veggies
- Quinoa salad with cucumber, olive oil, and lemon
- Smoothies made with Greek yogurt, banana, and almond milk
Keeping a food diary can help identify what works best when appetite fluctuates.
Medication & Supplements: Ask the Pharmacist
During pregnancy, every pill counts—especially for women managing celiac disease in Pregnancy. Gluten isn’t just hiding in baked goods; it can also appear in places you’d least expect—like prescription medications, over-the-counter supplements, and even certain prenatal vitamins. These hidden traces of gluten are often used as binders, fillers, or stabilizers in pills and capsules. The consequences of accidentally ingesting gluten during pregnancy go beyond an upset stomach. For women with celiac disease, even small exposures can lead to malabsorption of vital nutrients like folic acid, iron, and vitamin B12—nutrients critical to your baby’s brain development, neural tube formation, and growth.
So, how do you protect yourself and your child?
Here’s what every expectant mother with celiac disease in Pregnancy should do:
- Consult your pharmacist before starting any new medication — even if it’s over-the-counter. Pharmacists can confirm whether a specific brand or formulation is gluten-free.
- Don’t assume a supplement labeled ‘natural’ or ‘plant-based’ is safe—gluten can still be present in inactive ingredients or via cross-contamination.
- Stick to certified gluten-free prenatal vitamins, and avoid switching brands without checking ingredient lists.
Build a Strong Support Network
Managing celiac disease in pregnancy is not just a diet—it’s a lifestyle adjustment. Lean on professionals and community support to stay motivated and informed.
Build your team:
- A maternal-fetal medicine specialist
- A registered dietitian with celiac experience
- Celiac support forums or pregnancy-safe apps like Ovia and What to Expect
Real-Life Tip: Connect with other gluten-free mothers through local groups or online platforms. Shared experience can be a powerful motivator.
FAQs
Q1: Can I have a healthy pregnancy with celiac disease?
Yes, with early diagnosis and a strict gluten-free diet, a healthy pregnancy is entirely possible.
Q2: Can celiac disease cause miscarriage?
If untreated, yes. It can lead to miscarriage, preterm birth, and low birth weight.
Q3: What are early signs of celiac disease in pregnancy?
Fatigue, anemia, bloating, and unexplained weight loss or infertility are common.
Q4: Are prenatal vitamins safe for women with celiac disease?
Not all. Choose certified gluten-free supplements and ask your pharmacist to confirm.
Q5: Can my baby inherit celiac disease?
Celiac disease is genetic, but not all children of affected mothers will develop it.