Imagine waking up day after day feeling tired, thirsty, and not quite yourself. You brush it off, maybe it’s stress or just not getting enough sleep. For many people, these seemingly minor changes are the first whispers of a silent condition that affects over 1 in 10 adults worldwide: diabetes. What makes it especially dangerous is how quietly it can develop, often without dramatic symptoms, until severe damage has occurred. In this guide, we’ll unpack the key signs, root causes, and treatments for diabetes. Whether you’re newly diagnosed or supporting someone close, this could be your first real step toward clarity and control.
What Is Diabetes?
Diabetes is a chronic condition that affects how your body turns food into energy. When you eat, your body breaks down carbohydrates into glucose (sugar), which enters your bloodstream. Usually, the hormone insulin helps move that glucose into your cells. However, in diabetics, the body either produces insufficient amounts of insulin or is unable to use it efficiently, which results in elevated blood sugar levels.
Diabetes is a chronic health condition that occurs in two primary forms: mellitus and insipidus diabetes.
The more common type, mellitus, is further divided into Type 1 and Type 2. Type 1, often called juvenile or insulin-dependent diabetes, usually develops in children and young adults. In this form, the body is unable to produce insulin, a hormone essential for converting glucose from food into energy. Though less common, making up only 5–10% of all cases, Type 1 requires lifelong insulin therapy.
Type 2 diabetes, which accounts for 90–95% of all diagnosed cases, occurs when the body either doesn’t produce enough insulin or becomes resistant to it. Lifestyle factors, such as diet and physical activity, play a significant role in its development. While early stages can be managed through healthy habits, medications or insulin may be necessary over time. Unfortunately, many individuals remain undiagnosed due to subtle symptoms.
Diabetes insipidus, on the other hand, is a rare and unrelated condition. It stems from a deficiency of vasopressin, a hormone produced by the pituitary gland that controls fluid balance. This disorder causes excessive urination and intense thirst, as the kidneys are unable to conserve water properly.
Common Symptoms of Diabetes
At first, symptoms of diabetes may seem harmless or easy to misinterpret. Increased thirst and frequent urination, especially at night, are often among the first signs. Some people may start to notice unexplained weight loss, persistent hunger, low energy, and fatigue that persists.
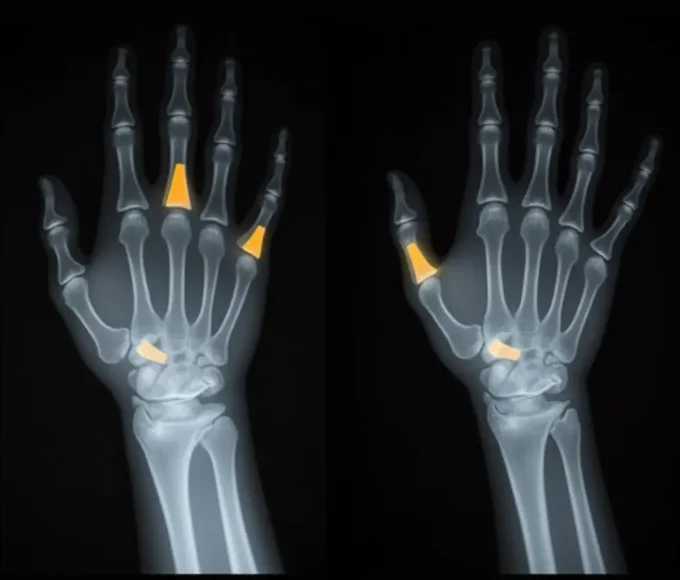
As the condition progresses, symptoms can become more noticeable. Blurred vision, tingling or numbness in the hands and feet, and slow-healing cuts or frequent infections may develop. In some cases, dark, velvety patches of skin, especially around the neck, signal insulin resistance. Type 1 symptoms tend to appear suddenly, while Type 2 creeps in over time.
Root Causes and Risk Factors
Each type of diabetes has its cause. Type 1 is triggered by an autoimmune response that destroys the pancreas’s ability to produce insulin. While the exact cause is unknown, it’s believed to be a combination of genetic and environmental factors. In contrast, Type 2 diabetes is most often tied to lifestyle: lack of exercise, poor diet, excess weight, and insulin resistance. Gestational diabetes arises during pregnancy due to hormonal changes that affect how insulin works.
Risk factors vary but often include being overweight, having a family history of diabetics, and being over age 45. Conditions like high blood pressure, high cholesterol, and polycystic ovary syndrome (PCOS) can also increase your risk. Recognizing these factors early can make all the difference.
How Is Diabetes Diagnosed?
Testing for diabetes is relatively straightforward and begins with a conversation with your healthcare provider. One standard method is the A1C test, which gives an average of your blood sugar levels over the past two to three months. A result of 6.5% or higher usually indicates diabetics.
Other diagnostic options include the fasting blood glucose test, taken after you haven’t eaten for several hours, and the oral glucose tolerance test, which measures your blood sugar response to a sugary drink. The latter is commonly used in screening for gestational diabetes. Early detection, particularly in high-risk individuals, is crucial for preventing complications.
Treatment Options: Medical and Lifestyle Approaches
Treating diabetics involves balancing medical support with daily lifestyle choices. For people with Type 1 diabetes, insulin therapy is essential. It’s delivered through injections or a pump to keep blood sugar levels in check. For Type 2, treatment may begin with diet and exercise, and progress to medications such as Metformin or insulin, depending on the individual’s case. Gestational diabetes is often managed through diet, but can also require insulin.
Beyond medication, lifestyle matters immensely. Choosing foods low on the glycemic index, prioritizing fiber and lean protein, and reducing processed sugar helps regulate blood sugar levels. Regular physical activity enhances insulin sensitivity. Monitoring blood sugar, whether with a simple finger prick or a continuous glucose monitor, enables people to stay in control.
Living Well with Diabetes
Managing diabetes is about more than just numbers; it’s about quality of life. People living with the condition thrive when they establish routines that include regular blood sugar checks, balanced meals, and physical activity. Just as vital is emotional well-being. Stress can disrupt glucose levels, so mindfulness practices, creative outlets, or simply talking to a counselor can be powerful tools.
Connection matters too. Support groups, whether in-person or online, can make a significant difference in one’s life. They provide a space to share struggles and celebrate progress. Regular doctor visits are equally crucial for monitoring eye health, kidney function, nerve damage, and foot health, especially for individuals with Type 2 diabetes.
Conclusion
Diabetics don’t have to define their lives. With proper knowledge, daily care, and a supportive network, it’s possible to manage the condition and live a vibrant life. Understanding the symptoms, uncovering the causes, and staying informed about treatment options are all critical steps on this journey.
If you’ve noticed signs or fall into a high-risk group, don’t wait. Talk to your doctor about screening. And if you’ve already been diagnosed, remember you’re not alone. The path ahead is one you can walk with confidence and support.
“So, what’s my final advice? Please don’t let a diabetes diagnosis define you. From my clinical experience, I can tell you that with the right knowledge, support, and a commitment to your health, you can live a vibrant, fulfilling life. By working with your doctor, making smart lifestyle choices, and connecting with a supportive community, you can manage your diabetes and thrive. Your health is a journey, and this is a path you can walk with confidence and control.”
Frequently Asked Questions
How do you deal with diabetes?
Managing diabetes involves a combination of healthy eating, regular exercise, monitoring blood sugar levels, taking prescribed medications or insulin, and managing stress effectively.
Is type 2 diabetes your fault?
No. While lifestyle factors like diet and activity levels can increase risk, genetics, age, and other uncontrollable factors also play a role in developing Type 2 diabetes.
What is a diabetic sugar level?
A normal fasting blood sugar level is below 100 mg/dL. A level of 126 mg/dL or higher on two separate tests typically indicates diabetics.
What are the 10 warning signs of diabetes?
Early signs include frequent urination, extreme thirst, unexplained weight loss, fatigue, blurred vision, slow wound healing, tingling in the hands and feet, constant hunger, dry mouth, and a higher risk of frequent infections.
How do I know if I’m diabetic?
If you’re experiencing symptoms or are at risk, ask your doctor for an A1C test, fasting glucose test, or oral glucose tolerance test to confirm the diagnosis.
How to avoid diabetes?
Prevention includes maintaining a healthy weight, eating a balanced diet, staying active, limiting excess sugar intake, quitting smoking, and getting regular check-ups, especially if you’re at risk.
Medically Reviewed by Dr. Muhammad Usman
References
- World Health Organization (WHO). Diabetes. Updated 2023. https://www.who.int/news-room/fact-sheets/detail/diabetes
- Centers for Disease Control and Prevention (CDC). What is Diabetes? Reviewed 2024. https://www.cdc.gov/diabetes/basics/diabetes.html
- American Diabetes Association (ADA). Standards of Care in Diabetes – 2024. Diabetes Care. https://diabetesjournals.org/care
- Mayo Clinic. Diabetes: Symptoms & Causes. Updated 2023. https://www.mayoclinic.org/diseases-conditions/diabetes
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). Diabetes Overview. Reviewed 2024. https://www.niddk.nih.gov/health-information/diabetes
- Harvard Medical School. Understanding Type 1 and Type 2 Diabetes. 2023. https://www.health.harvard.edu
- Johns Hopkins Medicine. Diabetes Basics. Updated 2023. https://www.hopkinsmedicine.org/health/conditions-and-diseases/diabetes